Project Outline: Investigating Gaps in the TB Care Cascade
Investigating the Reasons for Bad Outcomes Along the Care Cascade; A Qualitative Study
Supervisors: Dr. Ramnath Subbaraman, Pragya Dhar, Barbie Patel
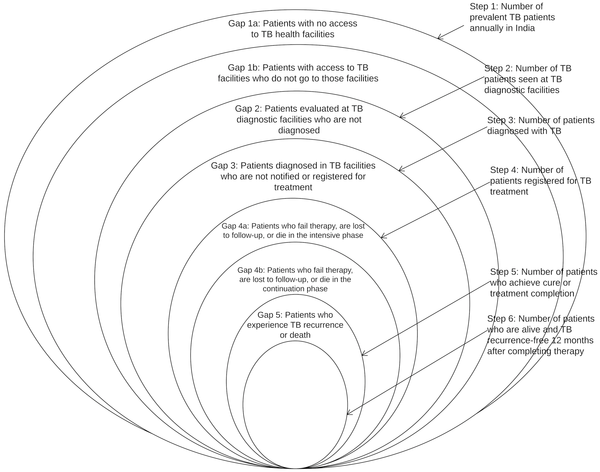
Tuberculosis is the world’s leading infectious cause of death, and India has an especially high burden of both incident cases and death when compared to the rest of the world. Previous research has shown that, despite there being infrastructures in place for tuberculosis treatment (namely the DOT program as implemented by the WHO), an unfortunate majority of people are not cured. There are several points of “drop-off” in care, including people who never make it to a clinic, those who are diagnosed incorrectly, etc. This is all outlined in a framework called the Tuberculosis care cascade, which highlights specific milestones a patient should be reaching to be cured.
Source: https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1002149
In India, TB is ideally treated through government centers, which have a specific testing and treatment protocol based on WHO standards. There is, however, a private sector that people often go to, which includes doctors with an MBBS (more Western medicine) and folk medicine providers. The care cascade is based on the government guidelines and we only have data on people who interacted with the government system at some point. However, many people move between both systems, so we are able to at least understand a portion of how people interact with both systems.
This study focuses specifically on people in gaps 4a, 4b, and 5, which are those who start but do not finish treatment or those who finished a full course but contracted TB again (called recurrence) or passed away. Many people who start treatment never finish it, because they pass away in the middle or for a variety of other reasons. The overarching goal of this research is to deeply examine these three gaps and understand what differences and similarities exist between each gap. By investigating the reasons causing people to fall into these gaps, we hope to understand what structural or systemic factors lead to these losses and whether these factors remain constant as we progress along the cascade. To understand exactly what these factors are, we are looking to see how patients interact with the healthcare system, which circumstances surrounding their life may have made it more difficult to get care, and how general perception of the disease affects both patients and healthcare workers. At the end of this study, we hope to have the information needed to fortify the TB care system to both retain existing patients and ensure new patients can make it through down the cascade
This study started in India, where Dr. Ram’s team used records of patients’ contact information that microscopy centers collected to follow up with them based on their treatment outcomes. Interviewees and their families were asked questions about the course of their treatment and what was going on when they stopped, including the following:
- Where they were getting the medication
- Costs of getting medication and general financial responsibilities
- Family responsibilities
- Behavioral habits (smoking, drinking, eating)
- Where they received care
- Quality of care questions such as:
- Whether TB diagnosis was communicated
- If healthy/ideal practices were communicated
- Wait times
- Attitude of staff
Currently, we are working on translating all the data from Hindi to English. As the interviews are being translated, we are also working on coding them with themes that people experience. This can range from broader societal issues, such as stigma or cultural norms to specific issues with the healthcare system, such as unclear communication of diagnosis. Once the interviews are coded, they will be statistically analyzed to find the most common issues and then used to target specific parts of the care cascade or TB care infrastructure that can be used to improve outcomes.
Please sign in
If you are a registered user on Laidlaw Scholars Network, please sign in