Project Outline: Immune Dysregulation and Parkinson's Disease Pathogenesis
Investigating Immune Dysregulation in Parkinson’s Disease Pathogenesis: An Integrative, Interdisciplinary Analysis via Multi-Omics and a Preclinical Model
Research Supervisor: Dr. Olga Rojas (MD, PhD)
Abstract
Parkinson's disease (PD) is widely accepted as a central nervous system disorder. However, it is being increasingly recognized in academia for its involvement in systemic immune dysfunction (Tansey et al., 2022). This project investigates how dysregulated peripheral immune responses contributes to PD onset and progression and aims to identify potential immune-related biomarkers as potential therapeutic targets for immunomodulatory solutions.
With over 12 million projected PD cases globally by 2040 (Feigin et al., 2019), early, disease-modifying therapies are imperative. Although current treatments largely focus on alleviating patient motor symptoms, growing evidence suggests immune cell activation, altered cytokine levels, and aberrant gene expression in the peripheral blood of PD patients (Tansey & Romero-Ramos, 2019). However, the specific immune pathways involved remain poorly understood. By characterizing these mechanisms, this project aims to help shift therapeutic strategies from symptomatic relief to precision-based disease modulation.
My research integrates multifaceted computational and experimental approaches. First, I’ll be analyzing transcriptomic datasets from peripheral blood mononuclear cells (PBMCs) and cerebrospinal fluid (CSF) of PD patients and healthy controls to identify differentially expressed immune-related genes. Using immune deconvolution tools, I will infer immune cell-type composition and identify dysregulated immune profiles. Second, I’ll validate key findings via a preclinical mouse model of PD, leveraging preliminary gut immune profiling data to assess translational relevance. Experimental validation in this project will include immunophenotyping and gene expression analysis of immune cell subsets. In combination, these approaches aim to reveal immune biomarkers and pathways that could inform future diagnostics or therapeutic strategies in PD.
Introduction
Parkinson’s disease (PD) is the second most prevalent neurodegenerative disease, and its prevalence is projected to double over the next 30 years (Dorsey, et. al, 2018). PD is characterized by the progressive loss of dopaminergic neurons in the substantia nigra, leading to motor symptoms such as tremors, rigidity, and bradykinesia. The main pathological feature is the accumulation of alpha-synuclein in the brain (Poewe, et. al, 2017).
PD is deeply personal to me; both of my grandfathers have been diagnosed with the disease, and one has passed away from it, exposing me to its profound impact. This drives my passion for uncovering its links to immune dysregulation. My fascination with the immune system, shaped by my own experiences with anaphylaxis, fuels my commitment to understanding its dual roles in protection and disease.
Emerging evidence links neuroinflammation, peripheral immune activation, and meningeal immunity to PD, potentially from its earliest stages, yet the underlying mechanisms remain unclear (Harms, et. al, 2021). This study integrates computational analysis of gene expression and single-cell data from cerebrospinal fluid (CSF) and PBMCs with experimental validation in a PD mouse model to investigate immune-related pathways.
Research Objectives & Questions
Objective 1: Identify immune-related pathways and biomarkers in Parkinson’s disease through computational analysis.
This study utilizes gene expression and single cell sequencing data to identify dysregulated immune pathways in PD. By analyzing PBMCs and CSF, we aim to uncover immune signatures linked to disease progression, clinical phenotypes, and neuropathology.
Objective 2: Validate key immune markers through pre-clinical experimental approaches.
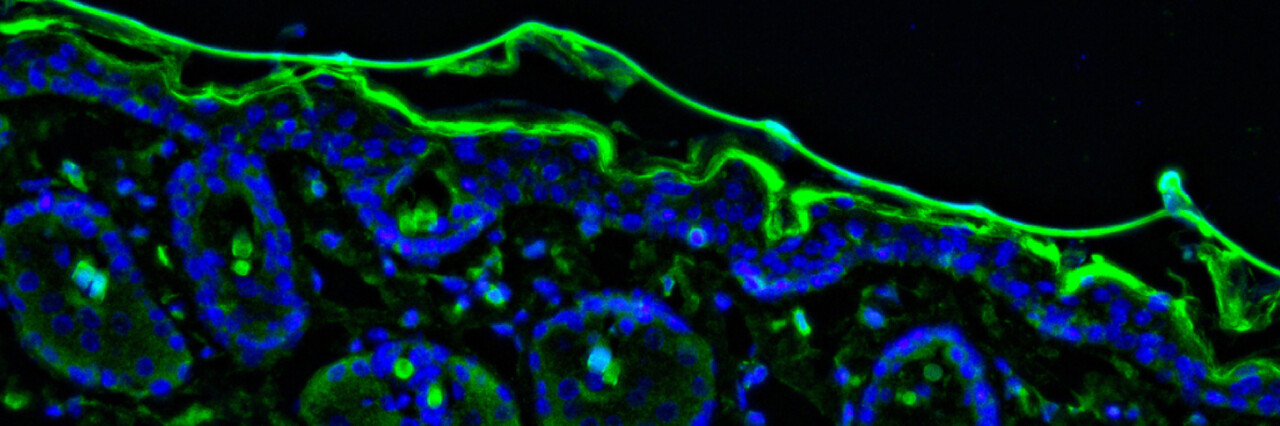
To validate computational findings, this study uses a well-established PD mouse model at Krembil Research Institute, where an AAV-A53T alpha-synuclein injection induces PD-like pathology. Immune profiling via flow cytometry, confocal imaging, ELISAs, and immunofluorescence, where appropriate, will assess immune responses in blood and meninges of PD mice. These approaches will reveal mechanistic links between meningeal immunity, neurodegeneration, and disease progression.
Primary and secondary research questions:
- What immune-related pathways and biomarkers are dysregulated in PD?
- What is the role of meningeal immune responses in PD pathogenesis?
- How well do immune-related findings from human PD data translate to preclinical models?
Background
Emerging research underscores the significant role of immune system dysregulation in Parkinson’s Disease (PD). Both central and peripheral immune responses have been implicated in PD pathogenesis, with studies highlighting microglial activation, T cell infiltration, and elevated pro-inflammatory cytokines in the brains of PD patients (Tansey & Romero-Ramos, 2019). Peripheral immune alterations, including changes in monocyte and lymphocyte populations, further suggest systemic immune involvement.
The gut–brain axis has also been compelling for its potential role in PD. Misfolded alphasynuclein, a hallmark of PD, has been detected in the enteric nervous system, indicating that pathological processes may originate in the gut and propagate to the brain via the vagus nerve (Klann et al., 2022). Gastrointestinal symptoms often precede motor manifestations, and studies have identified distinct gut microbiota profiles in PD patients, suggesting that gut dysbiosis may contribute to disease development (Klann et al., 2022), an intriguing future research endeavour.
These insights have influenced the direction of my research, which aims to integrate computational analyses of peripheral blood mononuclear cell (PBMC) and cerebrospinal fluid (CSF) transcriptomic data with experimental validation in a preclinical PD model. By identifying conserved immune signatures across human and animal models, this project seeks to elucidate the relationship between peripheral immunity and PD progression, potentially uncovering novel biomarkers and therapeutic targets.
Methodology
This project will employ a mixed-methods approach. The first phase of the project involves identifying immune-related gene expression changes in publicly available RNA sequencing (RNA-seq) datasets from peripheral blood mononuclear cells (PBMCs) and cerebrospinal fluid (CSF) cell samples of PD patients and healthy controls. Analysis will be conducted using R, employing tools such as DESeq2 for differential gene expression, and CIBERSORTx for immune cell deconvolution. Pathway enrichment analysis will be used to contextualize results within immune signalling networks.
Findings from the computational phase will inform wet lab experiments using the preclinical PD model. Experimental validation may involve RNA fluorescence in situ hybridization (RNA-FISH) and/or immunofluorescence as appropriate, in order to localize and quantify expression of key immune genes in peripheral tissues. Final methods will be determined in consultation with the lab based on antibody availability and tissue-specific resolution requirements.
All research activities will be conducted exclusively at the Krembil Research Institute (UHN) under the direct supervision of Dr. Olga Rojas, with mentorship from a senior MSc student and support from the broader lab team.
Training/Certifications Needed
Before beginning any experimental work, I will complete all required University Health Network (UHN) training modules. These include:
- WHMIS (Workplace Hazardous Materials Information System)
- Laboratory Biosafety Training
- Health and Safety Awareness for Ontario Workers
- Animal Care and Use Training
Online training completion is expected to take approximately 4-5 days total, including assessments and documentation. In addition to formal certification, I will also engage in hands-on protocol familiarization by shadowing a senior MSc student in the lab during the month of May. This will provide practical exposure to the experimental techniques and model systems used in the lab, complementing the online training.
Potential Impact
This research project addresses a critical question in neuroimmunology: how systemic immune dysfunction contributes to the development and progression of Parkinson’s Disease (PD). As the second most common neurodegenerative disorder worldwide, with rising incidence in aging populations, PD represents a growing global health challenge, and yet effective disease-modifying therapies remain elusive. By investigating conserved immune signatures across species and systems, this project aims to uncover novel insights into the role of peripheral immunity in PD pathogenesis.
The integration of computational analyses of publicly available human datasets with in vivo validation in a preclinical mouse model is a powerful, translational approach. It allows us to move beyond association and toward identifying actionable immune biomarkers or therapeutic targets. Understanding how immune dysregulation is reflected in accessible tissues like blood could revolutionize how we diagnose, monitor, and ultimately treat PD, potentially enabling earlier intervention and personalized immunomodulatory therapies for patients.
The broader implications of this research extend beyond PD. By contributing to a deeper understanding of neuroimmune interactions, the findings may inform research in other neurodegenerative conditions where inflammation plays a role, such as Alzheimer’s disease or multiple sclerosis. This work also underscores the value of open-access data and cross-disciplinary collaboration in driving biomedical discovery.
Ultimately, this project contributes to a greater global effort to investigate the complex association between the immune system and the brain, bringing us a step closer to developing more effective, patient-centred strategies for managing neurodegenerative diseases.
References
Chao, Y., Wong, S. C., & Tan, E. K. (2014). Evidence of inflammatory system involvement in Parkinson's disease. BioMed research international, 2014, 308654. https://doi.org/10.1155/2014/308654
Dorsey, E. R., Sherer, T., Okun, M. S., & Bloem, B. R. (2018). The Emerging Evidence of the Parkinson Pandemic. Journal of Parkinson's disease, 8(s1), S3–S8. https://doi.org/10.3233/JPD-181474
Feigin, V. L., Vos, T., Nichols, E., Owolabi, M. O., Carroll, W. M., Dichgans, M., Deuschl, G., Parmar, P., Brainin, M., & Murray, C. (2020). The global burden of neurological disorders: translating evidence into policy. Lancet Neurology, 19(3), 255–265. https://doi.org/10.1016/S1474-4422(19)30411-9
Harms, A. S., Ferreira, S. A., & Romero-Ramos, M. (2021). Periphery and brain, innate and adaptive immunity in Parkinson's disease. Acta neuropathologica, 141(4), 527–545. https://doi.org/10.1007/s00401-021-02268-5
Klann, E. M., Dissanayake, U., Gurrala, A., Farrer, M., Shukla, A. W., Ramirez-Zamora, A., Mai, V., & Vedam-Mai, V. (2022). The Gut-Brain Axis and Its Relation to Parkinson's Disease: A Review. Frontiers in aging neuroscience, 13, 782082. https://doi.org/10.3389/fnagi.2021.782082
Poewe, W., Seppi, K., Tanner, C. et al. Parkinson disease. Nat Rev Dis Primers 3, 17013 (2017). https://doi.org/10.1038/nrdp.2017.13
Tansey, M. G., & Romero‐Ramos, M. (2019). Immune system responses in Parkinson’s disease: Early and dynamic. The European Journal of Neuroscience, 49(3), 364–383. https://doi.org/10.1111/ejn.14290
Tansey, M. G., Wallings, R. L., Houser, M. C., Herrick, M. K., Keating, C. E., & Joers, V. (2022). Inflammation and immune dysfunction in Parkinson disease. Nature Reviews Immunology, 22(11), 657–673. https://doi.org/10.1038/s41577-022-00684-6



Please sign in
If you are a registered user on Laidlaw Scholars Network, please sign in