Exploring Collaborative Leadership at the Patient Engagement Open Forum

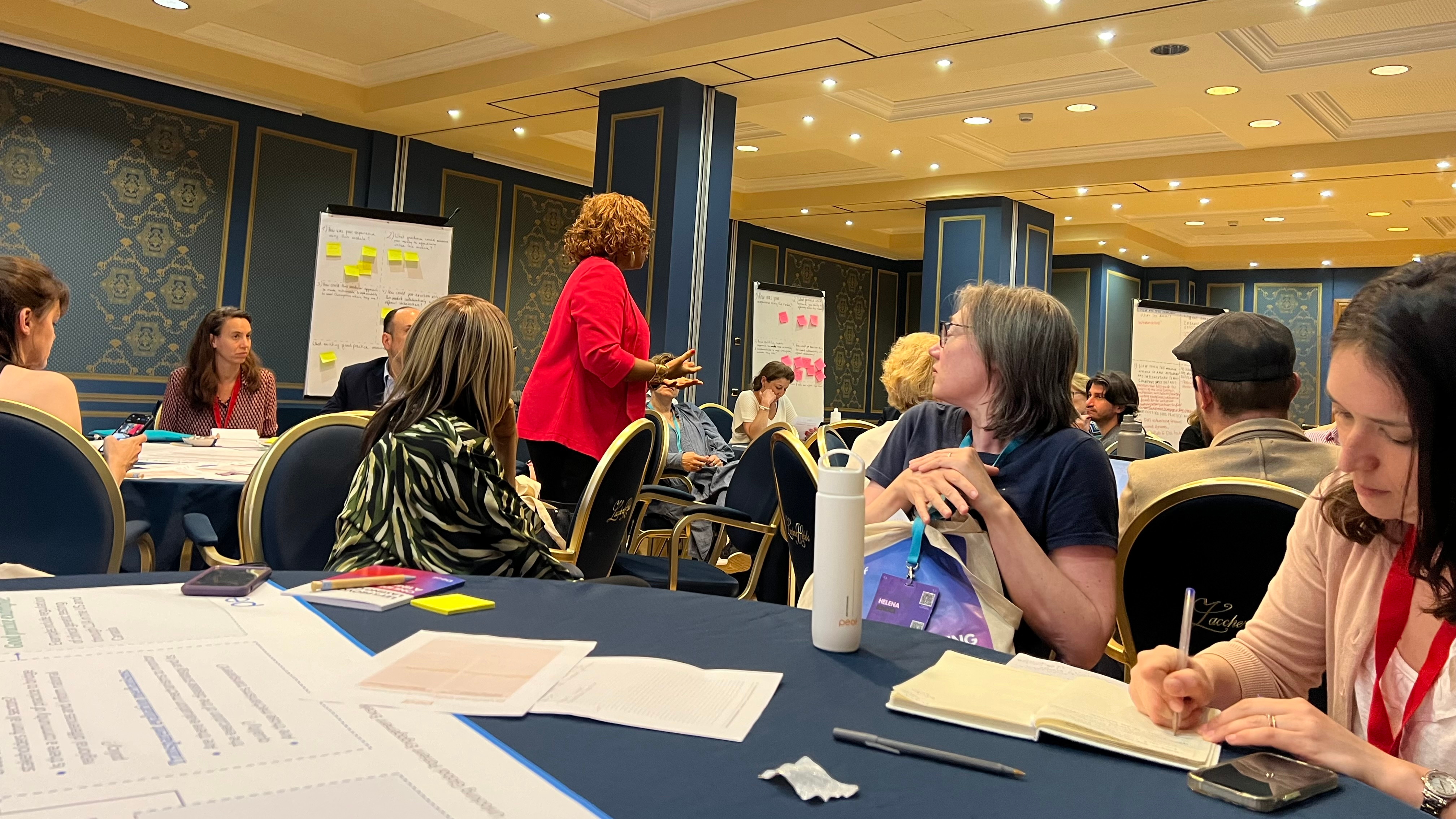
In May 2024, I had the privilege of attending and helping to facilitate various thought-provoking sessions at the Patient Engagement Open Forum (PEOF) in Baveno, Italy. Two of these sessions, "Seeding Success: Collaborative Crafting of Guiding Principles for Funding Agencies to Cultivate Early Patient Engagement" and "Driving Change: Testing Prototypes of Advocacy Roadmaps for Improved Access to Personalised Healthcare," provided a wealth of insights into collaborative leadership. Here’s what I learned about the power of bringing diverse voices together to drive change.

Seeding Success: Fostering Early Patient Engagement
The first session, "Seeding Success," focused on how research funders can support the early involvement of patients in research. This topic is close to my heart as it highlights the crucial role of patient voices in shaping meaningful research outcomes. The session brought together representatives from funding agencies, academia, patient communities, and industry to co-create guiding principles for early patient engagement. Key takeaways include:
- Diverse Voices, Unified Goals: The session showcased the strength of bringing varied stakeholders together. Researchers, patients, and funders each contributed unique perspectives, enriching the discussion and leading to more holistic recommendations.
- Education and Training: Emphasising the need for education and training for all involved parties—researchers, grant reviewers, and patients—the session highlighted that collective learning is crucial for understanding and valuing patient engagement.
- Sustainable Relationships: Building and maintaining relationships with patient communities was highlighted as crucial. This is not a one-time effort but an ongoing dialogue that enhances the research's relevance and impact.
It was inspiring to see how different stakeholders, each with their unique perspectives, worked together towards a common goal. This collaborative approach is vital in transforming grant funding to support early patient engagement effectively.

Driving Change: Advocating for Personalised Healthcare
The second session, "Driving Change," centred on developing advocacy roadmaps to improve access to personalised healthcare. Despite its potential, precision medicine (PM) is still not a reality for many patients due to various challenges, gaps, and barriers within the healthcare system. This project aims to tackle these obstacles and facilitate better access to PM by supporting champions who can influence system-level change.
The advocacy roadmaps developed in this session are designed to be modular, fit-for-purpose, and adaptable to various health systems. Here's a breakdown of how these roadmaps aim to support advocacy efforts:
- Identifying Access Barriers: The roadmaps help PM champions identify the specific barriers to accessing PM within their country's health system.
- Guidance on Advocacy: The roadmaps offer strategies on how to advocate effectively. This includes identifying key stakeholders, understanding their influence, and crafting compelling arguments to drive system-level action.
- Strategic Empowerment: PM champions are equipped with insights on how to assess their health system's readiness for personalised healthcare. The roadmaps guide them in understanding regulatory environments, healthcare budget allocations, reimbursement processes, care practices, workforce training, and digital infrastructure.
- Flexible and Actionable: Designed to be adaptable, the roadmaps account for different types of health systems, from high-income countries with advanced infrastructure to low- and middle-income countries with varying levels of readiness.
The collaborative spirit was again the cornerstone of this session. Participants worked together to refine a modular advocacy roadmap tailored to various health systems and stages of PM maturity.
This session was a testament to the power of collaborative leadership in addressing complex healthcare challenges. Participants from various stakeholder groups shared their experiences and insights, enriching the roadmap development process. The collaborative effort demonstrated how diverse perspectives can lead to more robust and effective advocacy tools.
Reflections on Collaborative Leadership
What resonated most with me throughout these sessions was the profound impact of collaborative leadership. Here are my key reflections:
Inclusivity is Powerful: Involving diverse stakeholders in discussions leads to richer, more comprehensive solutions. It’s a reminder that everyone’s voice matters and contributes to the collective wisdom.
Ongoing Learning: The dynamic nature of healthcare demands continuous learning and adaptation. Collaborative leadership fosters an environment where knowledge is shared, and strategies are continuously refined.
Building Trust: Trust is the foundation of any successful collaboration. Building and maintaining trustful relationships with patient communities and other stakeholders ensures sustained engagement and meaningful outcomes.

Moving Forward
As I left the Patient Engagement Open Forum, I felt inspired and empowered by the collaborative spirit I witnessed. The sessions highlighted the immense potential of collective efforts in driving meaningful change in healthcare. Stay tuned for my detailed report on the outcomes of these sessions, where I will delve deeper into the recommendations for supporting early patient engagement and improving access to personalised healthcare.
I would like to express my sincere gratitude to The Synergist and my supervisors Vincent Raske and Silvia Bornengo for their invaluable guidance and unwavering support throughout my Leadership-in-Action project. I would also like to extend my profound thanks to Lord Laidlaw and the Laidlaw Foundation for this incredible opportunity.





Please sign in
If you are a registered user on Laidlaw Scholars Network, please sign in